PLEASE NOTE: The information in this blog is for educational purposes only. It is not a substitute for professional medical advice. Consult your healthcare provider if you’re seeking medical advice, diagnoses, or treatment.
Have you ever been told to avoid or limit red meat for health challenges like heart disease, cancer, and even diabetes?
If so, you’ve probably heard the calls to avoid animal foods if you have gout, a painful form of arthritis that affects over 9 million Americans (1). Gout patients are often advised to limit their consumption of red meat, organ meats, and seafood.
But do these foods cause the extreme discomfort of a gout attack? Or are there missing links that are being overlooked?
Gout appears to have been described as early as ancient Greece, and despite being “well-understood,” the management of this condition often doesn’t lead to lasting relief (2).
This article will explore the background of gout, whether foods like red meat cause gout, and solutions to consider if you’re struggling with gout!
What is Gout?
Gout is the most common form of inflammatory arthritis globally, primarily occurring in men, racial minorities, and the elderly (3). It’s characterized by inflammation in joints, tendons, and surrounding tissues induced by monosodium urate (4).

In addition to being incredibly painful, gout often occurs alongside cardiovascular disease, chronic kidney disease, diabetes, and neurodegenerative diseases (5).
When left untreated, gout may result in chronic pain or irreversible joint damage (6).
The leading cause of gout is hyperuricemia, which is caused by increased formation or reduced excretion of uric acid (7, 8). However, most patients with hyperuricemia never develop gout.
Gout development has a strong genetic component but is also connected to age, obesity, diet, and certain medications (9).
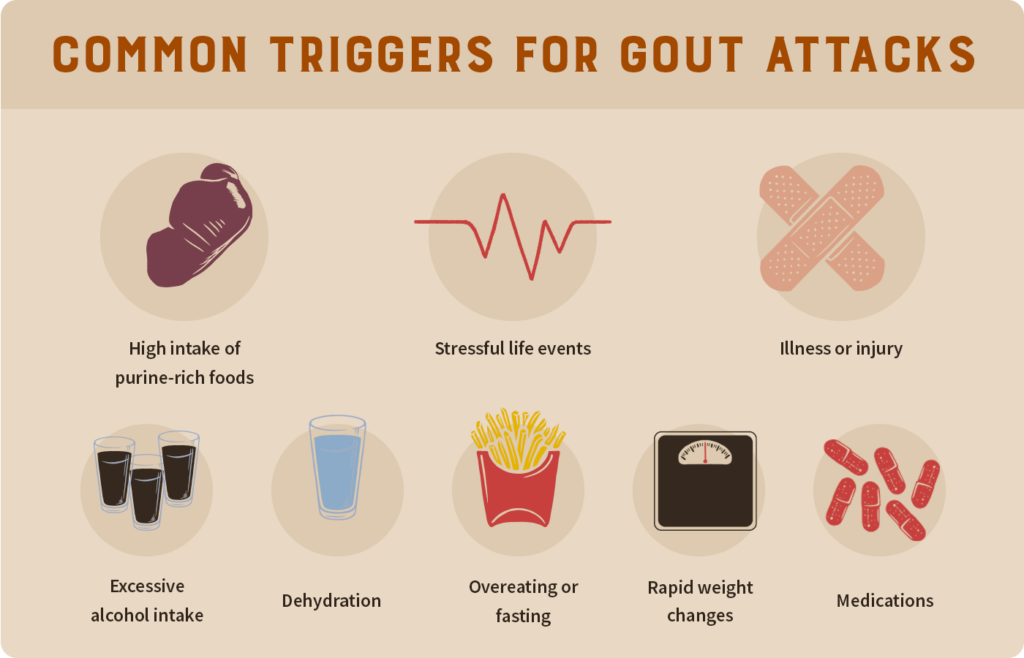
Flare-ups may occur from stress, diet choices, as well as from drugs like aspirin (10).
The Role of Uric Acid in Gout & Hyperuricemia
You can’t make it through a discussion on gout without hearing about uric acid, which is a natural antioxidant found in the human body (11). Uric acid forms after the breakdown of purines. Purines are a chemical found in alcohol, seafood, organ meats, and other foods.
Studies have suggested that uric acid may act as a “physiological alarm signal” during times of stress (12). Elevated levels of uric acid in the blood are also one of the best predictors of obesity, hypertension, and diabetes (13).
Both gout and hyperuricemia are related to the overproduction or underexcretion of uric acid. 70% of uric acid is excreted through the kidneys, while the intestines handle the rest (14).
The Impact of Diet on Gout
The exact impact of diet on the management of gout is controversial (15).
For example, the typical diets recommended for gout patients are Mediterranean, low-purine, and Dietary Approaches to Stop Hypertension (DASH). Each of these approaches presents different challenges!
The DASH diet is a plant-focused diet rich in nuts, seeds, fruits, vegetables, and lean meats to control hypertension. As of 2022, it was unclear if following the DASH diet alone leads to relevant improvements in gout (16).
The Mediterranean diet is another popular option that emphasizes olive oil, fish, plant proteins, whole grains, and a low intake of red meat. As with the DASH diet, there’s a lack of evidence among those with gout (17).
Lastly, the low-purine diet advocates avoiding organ meats, canned fish, shellfish, and alcoholic beverages, as these can contain higher purine levels. Strict purine restriction may not be effective for uric acid control and is often unsustainable (18).

To add even more confusion, both plant-based and meat-rich diets can lead to elevated uric acid levels.
One study examined the uric acid levels of meat and fish eaters, vegans, and vegetarians. Those on a vegan diet had the highest uric acid concentrations, while vegetarians (who ate fish but not meat) had the lowest concentrations (19).
Plus, the guidance to avoid purine-rich foods is based on increased serum uric acid in animals or humans fed purified purine (20).
Does Red Meat Cause Gout?
While meat and organs may contribute to gout flares, removing them from your diet doesn’t address the root causes.
As Paul Saladino, MD, explains in multiple videos on gout, he (and many others) eats large quantities of meat, organs, and fruit, yet he has a low uric acid and has never developed gout.
So why do some people experience gout attacks when eating meat and organs?
The missing variable in the equation appears to be metabolic health status, as underlying metabolic dysfunction and pathologic insulin resistance play a significant role in inflammation and impaired uric acid metabolism (21).
Individuals with chronic diseases like diabetes, hypertension, obesity, or chronic kidney disease have higher incidences of gout (22).

Insulin resistance resulting from obesity can reduce the excretion of uric acid, leading to hyperuricemia. Similarly, hypertension (high blood pressure) can limit uric acid excretion and contribute to gout development (23).
If you’re metabolically unhealthy, you may struggle with the purine content of meat and organs, but deeper issues may be present.
Common Yet Overlooked Causes of Gout
Meat, organs, and fructose tend to get most of the attention for gout. But there are numerous other contributing factors to be aware of!
As with many health challenges, some individuals have a genetic predisposition to gout. There’s a saying that “genetics load the gun, but diet and lifestyle pull the trigger.” This appears to be the case with gout.
A study from 2022 concluded that a healthy lifestyle “can counteract a high genetic predisposition for gout and that individuals with a low genetic predisposition for gout can lose their inherent protection if they have an unfavorable lifestyle. (24)”
Alcohol intake, obesity, and the use of certain medications are other factors that can impact your risk of developing gout (25).

Obesity can increase uric acid and appears to be a main driver of hyperuricemia (26, 27). One study found that 91% of gout cases in their cohort occurred in men with a BMI of 23 or higher (28). So, gradual weight loss is commonly suggested for gout patients.
Aspirin may lead to decreased uric acid secretion or increased reabsorption, elevating uric acid levels (29). Medications, such as diuretics, have also been connected to gout (30).
Many studies report that alcohol intake increases the risk of developing gout (31). Once again, it may interfere with uric acid excretion (32).
Heavy metal exposure and gut health are emerging areas of interest for gout research.
Heavy metals can enter the body through different pathways (such as food and water) and negatively impact human health (33). It’s been shown that workers exposed to lead have higher serum uric acid levels and occurrences of hyperuricemia compared to a control group (34).
Like so many other health challenges, gut dysbiosis may contribute to gout (35).
To make things more interesting, NSAIDs are commonly prescribed drugs to treat gout. One of the potential side effects is gastrointestinal damage (36).
As you can see, the possible contributors to gout are quite extensive and go beyond just meat consumption or genetics!
8 Diet and Lifestyle Strategies to Improve Gout
Both gout and hyperuricemia can respond positively to changes in diet, lifestyle, or medication (37). Like so many modern health challenges, your quality of life doesn’t have to suffer after a diagnosis such as gout!
Here are some main takeaways to consider if you’re struggling with gout (38, 39, 40):
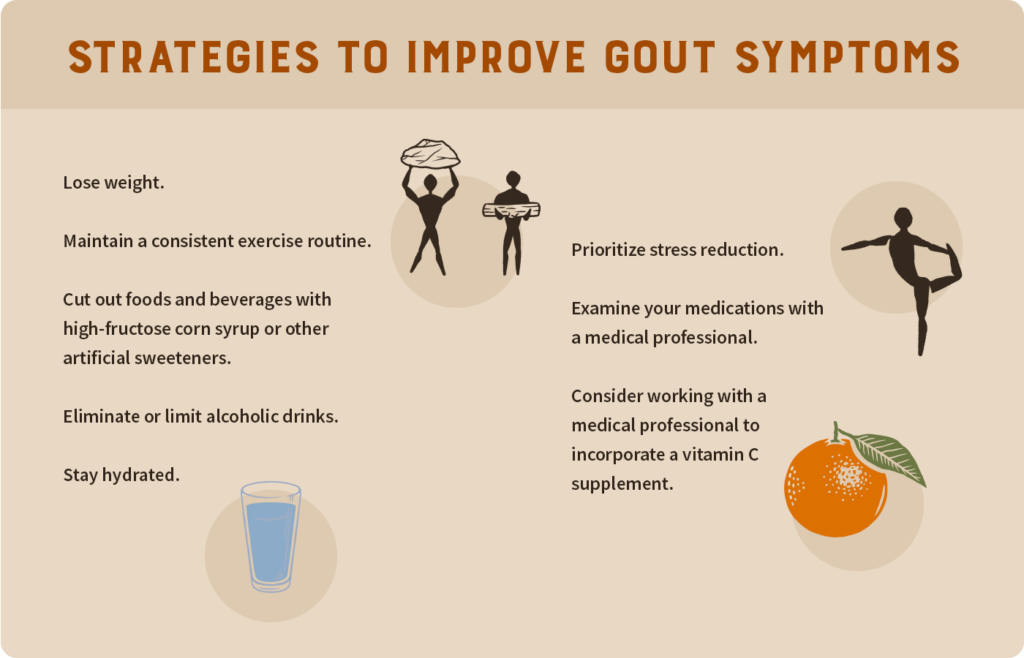
Discuss these steps with a medical professional before making any significant changes.
The Animal-Based Diet & Gout: Are They Compatible?
What should you do if you’re interested in the animal-based or carnivore diet but have gout?

As you may have seen, the animal-based diet primarily consists of well-raised meat and organs, fruits, honey, dairy, and other low-toxicity foods.
In epidemiological studies, red meat and organs are regularly associated with gout development and can be high in purines (41). The very nature of these studies is that they cannot prove causation. So, people with gout may be consuming meat, but it doesn’t necessarily mean it’s the true cause.
Fructose (a form of sugar in fruits and some vegetables) is another point of emphasis when discussing gout, as it may raise uric acid levels (42). Despite containing fructose, fruits are viewed as “likely safe” against gout flares, while the impact of fruit juices is less certain (43).
Dairy products are thought to lower concentrations of uric acid (44).
Again, it’s best to work with a medical professional before making major changes to your diet!
Promote Healthy Weight Management
Metabolism. Energy. Drive.
Meat Causes Gout, Right? It’s Not That Simple!
Gout is incredibly uncomfortable to deal with, yet conventional treatments often fall short.
Like many health challenges, gout has a genetic component but is also impacted by diet, lifestyle, and environmental exposures.
The idea that purine-rich foods (such as red meat) cause gout appears oversimplified. Metabolic health, alcohol intake, gut health, and even the use of certain medications can play a role as well.
It’s easy to feel stuck with a diagnosis like gout, but the reality is that diet and lifestyle adjustments can result in dramatic improvements in your quality of life!
Subscribe to future articles like this:
