Vitamins are essential nutrients. We eat them in foods (think vitamin C), or our bodies synthesize them (think vitamin D) through various biological mechanisms.
The idea of “vitamin toxicity” may sound like an oxymoron, it’s believable to many because it’s consistent with the principle of ‘the dose makes the poison.’
Vitamin A toxicity is especially prominent in Western medicine due to the narrative that suggests it can increase the risk of birth defects in pregnant women. However, there’s also evidence that increasing Vitamin A consumption can lower the risk of birth defects. So what’s the truth?
We’re here to set the record straight on vitamin A and provide some recommendations for how to get the right amount in your diet, whether you’re pregnant, want to conceive, or just want to feel better.
What this article covers…
- What is Vitamin A toxicity?
- Optimum Vitamin A levels
- The truth about Vitamin A toxicity and pregnancy
What is Vitamin A Toxicity?
Vitamin A is a fat-soluble, essential nutrient that your body acquires through your diet. Some foods contain vitamin A as “preformed” vitamin A, meaning your body can use it directly. Other foods contain provitamin forms, known as carotenoids (e.g., beta carotene), which your body transforms into vitamin A.
In studies, toxicity is almost always connected to preformed vitamin A, as a synthetic compound, or in foods where it is found at ultra-high concentrations (e.g., polar bear liver).
Since it is fat-soluble, excess vitamin A accumulates in your fat tissues, where it can cause symptoms such as headaches, nausea, skin disorders, and blurred vision. Excess vitamin A has also been linked with birth defects, although the research is contradictory and deserves a more thorough explanation. More on that later…
When consuming the provitamin form, your body is able to process what it needs and shed the excess. It is technically possible to overdose on carotenoids, resulting in a yellowing of the skin, but this condition is harmless and dissipates on its own if you stop consuming the excess vitamin.
There are some indications that smoking and consuming excess provitamin A can increase your risk of lung cancer — the scientific literature on this issue is inconclusive.
In most cases, vitamin A toxicity is caused by consuming too much preformed vitamin A (e.g., retinol, retinyl palmitate, retinyl acetate). On the other hand, there is actually a fairly wide dosage that is considered healthy and safe, even during pregnancy. Your goal should be thoughtful consumption of vitamin A, especially if you use supplements that contain significant doses of preformed vitamin A.
Let’s dive deeper…
Optimal Vitamin A Levels Vary Widely
Humans need vitamin A at every stage of life, from fetuses to old age. Vitamin A supports your vision, immune system, hormones, reproductive functions, and allows your heart, lungs, and vital organs to work properly.
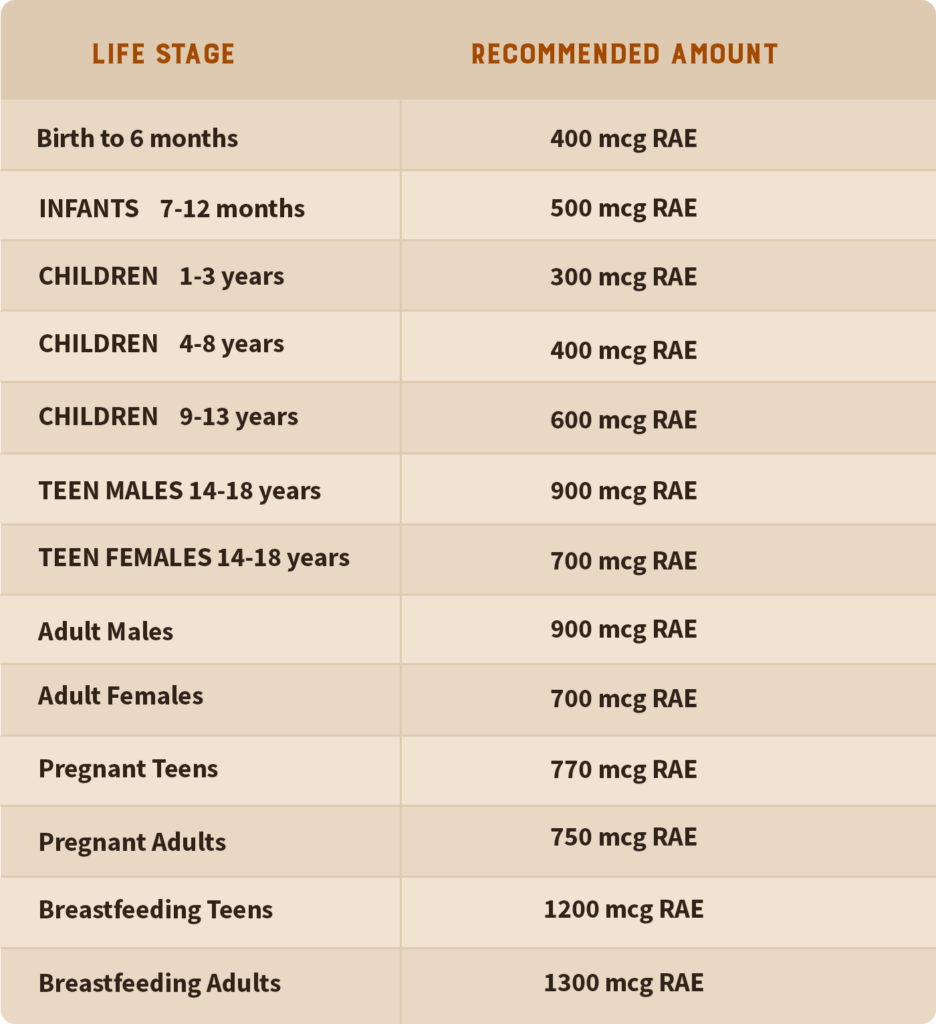
The recommended daily allowance (RDA) of vitamin A is currently measured in micrograms of retinol-activity equivalent (mcg RAE). You will still see it measured in IU (international units) in academic research, internet discussions, and even on some supplement labels. The mcg RAE metric is meant to compensate for the two classes of vitamin A (preformed and provitamin) and how your body processes them — essentially, how much of the substance is available for your body to use after it’s been ingested/metabolized.
Remember:
- Provitamin A is a precursor to the form of vitamin A that your body can uptake without processing. It is technically not as bioavailable, but the benefit is that your body sheds the excess. It’s very hard to reach toxicity with forms of provitamin A, such as beta carotene.
- Preformed vitamin A is the type your body can use immediately, making it highly bioavailable. It is the type most associated with toxicity due to its abundance in fortified foods and popularity in health supplements.
We realize that it can be difficult to keep the terms and units of measurement straight, so we’ll make it as clear as we can. We’ll also discuss vitamin A deficiency, acute toxicity, and chronic toxicity so you have a better idea of what the dangers are.
Too Little: Vitamin A Deficiency
Because humans acquire vitamin A through their diets, deficiency is most common in developing countries where people do not have access to foods rich in vitamin A or lack awareness of its importance. The majority of the US population, and populations in other developed countries, have access to foods that are naturally rich in vitamin A, in addition to fortified foods, such as breakfast cereals and milk, containing extra preformed A — the type your body can use immediately (1).
Symptoms of vitamin A deficiency include poor vision, especially at night. If left untreated, it can lead to permanent blindness. Chronic deficiency is connected with poor respiratory development and disease. It’s also a co-factor in diseases such as measles and infection-associated diarrhea — leading to increased severity and death from these diseases (2). Again, these situations are most common in poor countries where undernourishment prevails.
There are also health conditions that prevent your body from absorbing vitamin A. These are connected with your body’s ability to process fat and include pancreatic malfunction and gastrointestinal disorders.
In short, even if you’re eating a conventional Western diet, your risk of consuming too little vitamin A is very low. However, at Heart & Soil, we feel that a diet high in fortified foods (usually processed, grain-based foods) is problematic for other reasons. We suggest getting your vitamin A from animal-based sources, where it is highly bioavailable and free from other toxic compounds (such as you find in many plant foods).
Too Much: Acute Vitamin A Toxicity
Preformed vitamin A is fat-soluble, and your body stores it in fat tissues. Acute toxicity happens when you’ve consumed an extremely high amount over a short period of time, and symptoms manifest in a matter of days or weeks.
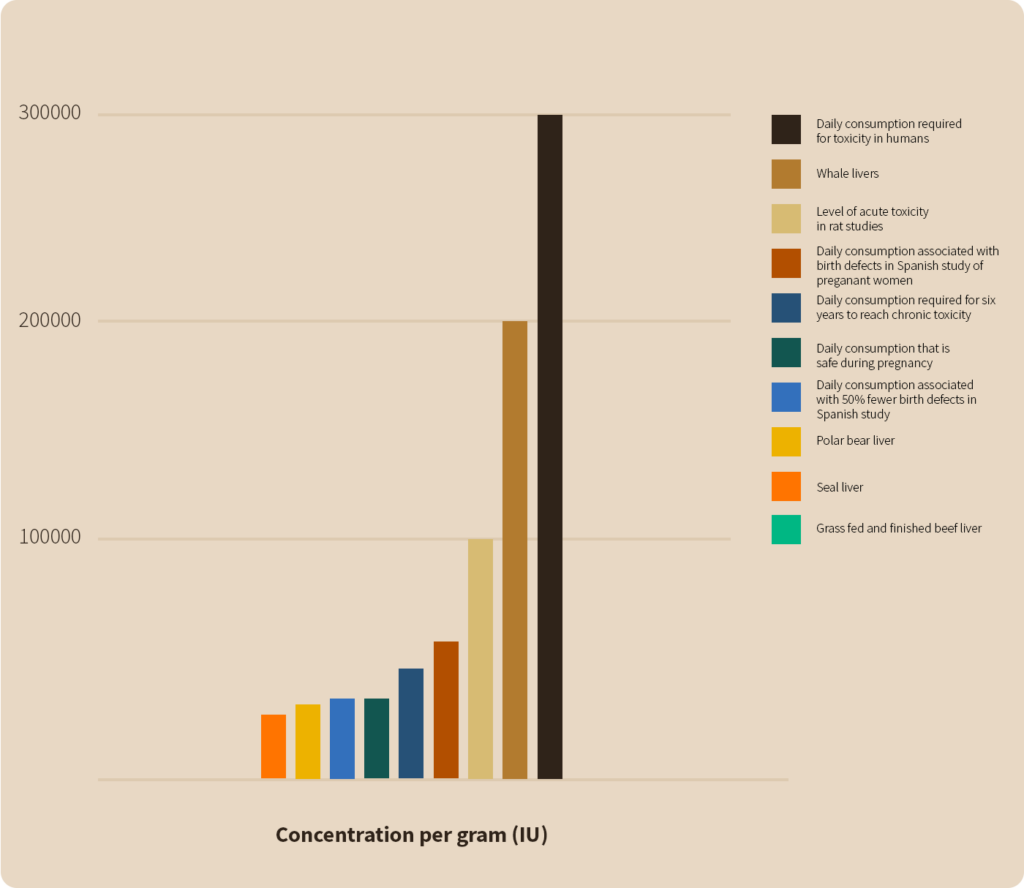
In fact, the major concern around vitamin A toxicity originated with arctic explorers who consumed polar bear liver, which contains 153,900 mcg RAE per ounce. That’s 171 times the daily recommended intake for an adult human male! Researchers examined the phenomenon of vitamin A toxicity in rats and discovered that 100,000 IU (30,000 mcg RAE) resulted in acute toxicity (3).
Outside of consuming rare foods such as seal, polar bear, and whale liver or ingesting high levels of synthetic retinol, it would be difficult to accidentally consume enough vitamin A to cause acute toxicity.
Too Much for Too Long: Chronic Vitamin A Toxicity
The greater concern is with sustained consumption of high doses of vitamin A resulting in chronic toxicity. Chronic toxicity can build up over years by ingesting nominally high daily doses of vitamin A (25,000 IU or 7,500 mcg RAE) or over a matter of months by ingesting much higher daily doses of 100,000 IU (30,000 mcg RAE). You would need to eat 3.5 ounces of liver every day for six years or 14 ounces of liver every day for six months to reach chronic toxicity.
In the paper (4) most often cited for this phenomenon, they used pigs as a model for humans due to the similarity in our digestive tracts, but this may be oversimplified. Subsequent studies established that synthetic vitamin A metabolizes differently than vitamin A as found in liver meat. Other vitamins and minerals such as D, K2, and zinc regulate Vitamin A metabolism — meaning that multiple deficiency co-factors can increase your likelihood of becoming toxic with vitamin A.
The Right Amount: Healthy Vitamin A Consumption
You need regular vitamin A in your diet. And finding the right amount can feel tricky. Especially for women who are pregnant, when demand for vitamin A is at its highest, and the secondary effects of overdosing (i.e., birth defects) are irreversible. We’ll tackle some of the research around vitamin A and pregnancy in the next section.
So, what’s the recommended daily allowance (RDA) of vitamin A?
For the majority of the population, consuming 2194 mcg RAE (eq. to 7313 IU) of retinol a day is well within the safe range. If you’re following an animal-based diet, this would be equivalent to 0.5-1 ounces of fresh beef liver a day.
Beef Organs
Nature's Ultimate Multivitamin
For comparison, a dose of Heart & Soil’s supplements* containing liver, such as Beef Organs and Pure American Liver holds the equivalent of 0.1-0.5 ounces of grass-fed, grass-finished beef liver. You’ll also get other critical nutrients such as zinc, selenium, B12, folate, riboflavin, and many others that support your metabolism, immune function, and nervous system.
*Estimated vitamin A content for our products can be found in Cronometer or by emailing us at [email protected]
The Truth About Vitamin A and Pregnancy
Here’s where the discussion of vitamin A toxicity reaches its highest stakes: How much vitamin A is safe to consume during pregnancy? Is the fear around vitamin A toxicity during pregnancy warranted? Wouldn’t it just be better to err on the low side?

As with many issues raised by scientific studies, this one deserves careful consideration.
A 1995 study led by Dr. Rothman of Boston University followed almost 23,000 women who consumed 10,000 IU or more from supplements or food sources (mainly from fortified breakfast cereals or processed food) during their first trimester and noted an increase in birth defects.
However, this study did not demonstrate an occurrence of birth defects ANY higher than the generally accepted rate of 3-4%. That means that no significant increase in birth defects could be attributed to the consumption of vitamin A in supplements or food. How this study became the go-to source for highlighting the dangers of vitamin A consumption during pregnancy is a mystery. The result is a “nothing burger” and pales in comparison to subsequent research proving the importance of vitamin A during pregnancy:
- A 1990 study on 25,000 births in Spain noted that doses of vitamin A over 40,000 IU (13,500 mcg RAE) daily carried a 2.7-fold higher risk of birth defects. Amounts of vitamin A up to 20,000 IU (6,000 mcg RAE) or between 20,000 and 40,000 IU both had a 50 percent lower risk of birth defects compared to no supplementation (5).
- A 1996 study of 522,601 births found that the children of women supplementing with at least 10,000 IU (3000 mcg RAE) of vitamin A alongside a multivitamin had a lower risk of birth defects than those of women who did not supplement. However, the association could not be distinguished from the effect of chance (6).
- A 1997 study of 1,508 births found no relationship between birth defects and using vitamin A supplements, including organ meat such as liver or fortified breakfast cereals (7).
- A 1999 prospective study of 423 mothers who consumed between 10,000 and 300,000 IU (3000-90,000 mcg RAE) of vitamin A in the first trimester compared to a group that did not supplement with vitamin A found no evidence of an increased risk of major malformations with increasing doses. The median dose was 50,000 IU (15,000 mcg RAE). The group as a whole had a 50 percent lower risk of major malformations than those who did not supplement. There were no significant malformations in offspring born to mothers consuming more than 50,000 IU (15,000 mcg RAE)(8).
As Chris Masterjohn, Ph.D., stated in an article from the Weston A. Price Foundation, “The preponderance of the evidence clearly favors the view that 20,000-25,000 IU (6,000-7,500 mcg RAE) of vitamin A during pregnancy is safe and may even reduce the risk of birth defects” (9).
If you would like to learn more about how Heart & Soil supplements can fit into your pregnancy health regimen, check out our blogs on pregnancy and breastfeeding.
Hopefully, this deep dive into vitamin A toxicity has given you a better understanding of the dangers of vitamin A toxicity and why the majority of people following a healthy animal-based diet are in no danger at all. Of course, our hope is to empower you with information so that you can take full ownership of your health and rely on your best judgment. Cheers to your radical health!
Subscribe to future articles like this:
